If you were asked what industry encounters the most violence in the workplace today, what would you guess? It’s not convenience stores, banks, or construction and manufacturing. All of these industries combined don’t see as much violence as healthcare does.
Healthcare and Social Service Workers Face Risk Every Day
Every year there are more attacks on healthcare and social service workers than any other field. 
- In 2013, over 70% of all workplace assaults occurred in healthcare and social service. That’s nearly three-quarters of all violence-related injuries, in an industry that employs less than 12% of all workers.
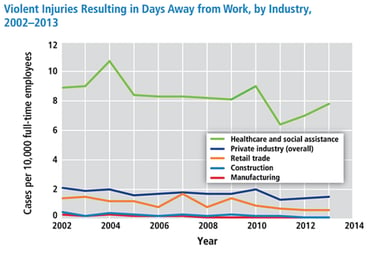
- In 2013, healthcare professionals experienced 7.8 cases of serious workplace violence injuries per 10,000 full-time equivalents (FTEs). Other large sectors had fewer than two cases per 10,000 FTEs.
- 21% of registered nurses and nursing students were physically assaulted and over half were verbally abused in a 21-month period
- 12% of ER nurses have experienced physical violence and 59% experienced verbal abuse during a seven-day period
- 13% of VA hospital staff have been assaulted in a year
The statistics on deaths due to violence are less encouraging: While fatal workplace violence has decreased in the last decade, homicides in healthcare have remained fairly steady—and in one sector, shooting deaths increased from 2000-2011.
(graph courtesy of OSHA 2015 Workplace Violence in Healthcare: Understanding the Challenge.)
These figures only account for serious injuries—injuries requiring time away from work for treatment. The numbers climb when non-serious injuries are included. And when you consider the fact that attacks are underreported, the situation becomes staggering.
Causes of Workplace Violence in Healthcare
Why so much violence in healthcare? It becomes clearer when you understand the factors that set the stage.
Eighty percent of violent attacks in the healthcare industry are perpetrated by patients. Other clients or customers account for 12% of attacks, and coworkers, visitors, and students are contributors as well.
Of all the sectors in healthcare, psychiatric aides are most vulnerable to attack, with a 10x higher likelihood than the next highest-risk group: nursing assistants. High-risk areas include emergency departments, geriatrics, and behavioral health.
When you consider the physical and psychological condition of many patients in a healthcare facility, and the stresses that staff are under, it’s easy to understand why the industry experiences so much violence. Some contributing causes include:
- Prematurely releasing injured and mentally unstable patients (due to insurance requirements)
- Presence of narcotics, which attracts addicts
- Patients injured from a fight continue to be aggravated
- Patient (or coworker) frustration at facility and insurance policies
- Understaffing
There are cultural factors at play, as well. Because healthcare staff tend to have an ethical conviction to “do no harm” to patients, some will knowingly risk their personal safety to help a patient. Others feel the need to protect their attackers from the stigma associated with certain illnesses, so incidents go unreported and unaddressed.
Physical space plays a role as well. Clinics and other healthcare facilities are often designed to maximize patient access and emphasize a caring environment. It also means aggressive patients and narcotic addicts have more opportunities to assault healthcare staff.
The Cost of Violence in Healthcare
According to OSHA, workplace violence is costly to staff and to the facilities where they work. Assaulted employees have to deal with physical and emotional fallout, and full recovery can take much longer than physical healing. Time off work can have financial and psychological impact, but returning to the place of the attack can also be a traumatic event.
While the emotional effects of workplace violence can’t be quantified, the costs on the healthcare industry are significant. A single serious injury can mean thousands of dollars in workers’ compensation and thousands of dollars in additional costs for overtime, temporary staffing, or recruiting and training a replacement.
Violent attacks can also lead to hidden costs such as higher turnover, lower morale, and reduced quality of care. For example:
- Caregiver fatigue, injury, and stress are correlated to increased medication errors and patient infections.
- Nurse dissatisfaction and burnout are reflected in patient satisfaction ratings.
- Injuries and stress lead some staff to leave the profession. Replacing a nurse can cost as much as $103,000.
What Can You Do About Violence in Your Facility?
Awareness of the issue is increasing. OSHA published Guidelines for Preventing Workplace Violence for Health Care & Social Service Workers in 1996, 2004, and 2015. The Joint Commission has also published a document about preventing violence in the healthcare setting. Voices across the industry are weighing in on best practices to prevent violence in clinics and facilities, and there are many possible initiatives that administrators must consider:
- Armed security staff
- Staffing with off-duty police
- Metal detectors
- Security cameras
- More restricted access for visitors and patients
- Security check-in stations
- Bulletproof glass installations
- Active shooter training and drills
Unfortunately, there’s no clear best practice—every healthcare setting is unique, and you’ll need to weigh the options for yourself. But Health Facilities Management provides helpful guidelines that can help you evaluate your security options.
Do a professional audit of your security
Evaluate your current security system, policies and procedures, training, and physical plant. Don’t rely on your own team to conduct the survey. You’ll need a credentialed, third-party professional who can give you a thorough and knowledgeable assessment.
Conduct a workplace violence policy assessment
Make sure your policy is up to date, fully backed by executive leadership, and effective. Use OSHA’s guidelines and other resources to guide your evaluation. Verify that the policy is accessible to all staff and thoroughly communicated throughout your organization.
Assemble a threat management team
This is a team of legal, security, HR, and psychiatry professionals, as well as local law enforcement. The threat management team is trained to spot potential threats and respond appropriately to mitigate danger in the workplace.
Flag dangers in the EHR
Whenever a patient or family member presents signs of being a potential threat, the attending healthcare professional should immediately flag it in the electronic health record. Develop policies and procedures to identify and deal with threatening patients and visitors, and those with violent criminal records. Any previous altercations with healthcare staff should be noted in the EHR so that future caregivers can take appropriate precautions.
Consider bulletproof features when designing your space
Any time your facility undergoes construction or remodeling, identify opportunities to upgrade the security of the building as well. This may include bulletproof barriers, electronic security systems, metal detectors, or more.
Train your staff to deal with workplace violence
This is an essential element in preventing workplace violence. Your staff must have thorough training in crisis intervention and security policies and procedures. Consider active shooter training and response protocol training as well.
The trend of violence in the healthcare industry can feel overwhelming. But with the help of security experts, you can initiate a solution that keeps your facility safe.
Next Steps:
- Sign up for our newsletter to stay up-to-date with the latest industry news
- Follow us on Twitter, Facebook or LinkedIn
- Download our Ultimate Guide to Bulletproof Glass and Bullet Resistant Barriers infographic

